The AI & Healthcare Opportunity
Part Two of How AI Can Help Improve the US Healthcare System
I’ve been talking about the importance of AI applications for a while now. IF we believe AI will be as transformative as everyone thinks, and IF we believe the hundreds of billions of infrastructure investments will see a positive ROI (or even something close to it), then we have to believe in the growth of AI applications.
Translated: we have to believe in AI’s ability to solve real problems and build companies around solving those problems.
So I’ll be doing a series of deep dives on AI applications starting with one of the biggest problems our country faces: the state of US healthcare. It’s becoming prohibitively expensive, weighed down by complexity, bureaucracy, and the ensuing administrative burden on providers (and in turn, patients).
It’s a problem that touches all of us, and it’s a problem technology is so well suited to solve.
This article is my best attempt to explain (1) why I’m so excited about AI in healthcare, (2) the state of healthcare software, (3) the state of healthcare & AI investments, (4) the areas where AI can help most, and (5) my thoughts on what it will take to make the impact I’m so excited about.
By no means is it perfect, but I do hope it starts a conversation. If you’re interested (as a builder or buyer of these tools) to be part of that conversation, feel free to shoot me a message.
Let’s get to it.
I. The US healthcare system is ailing.
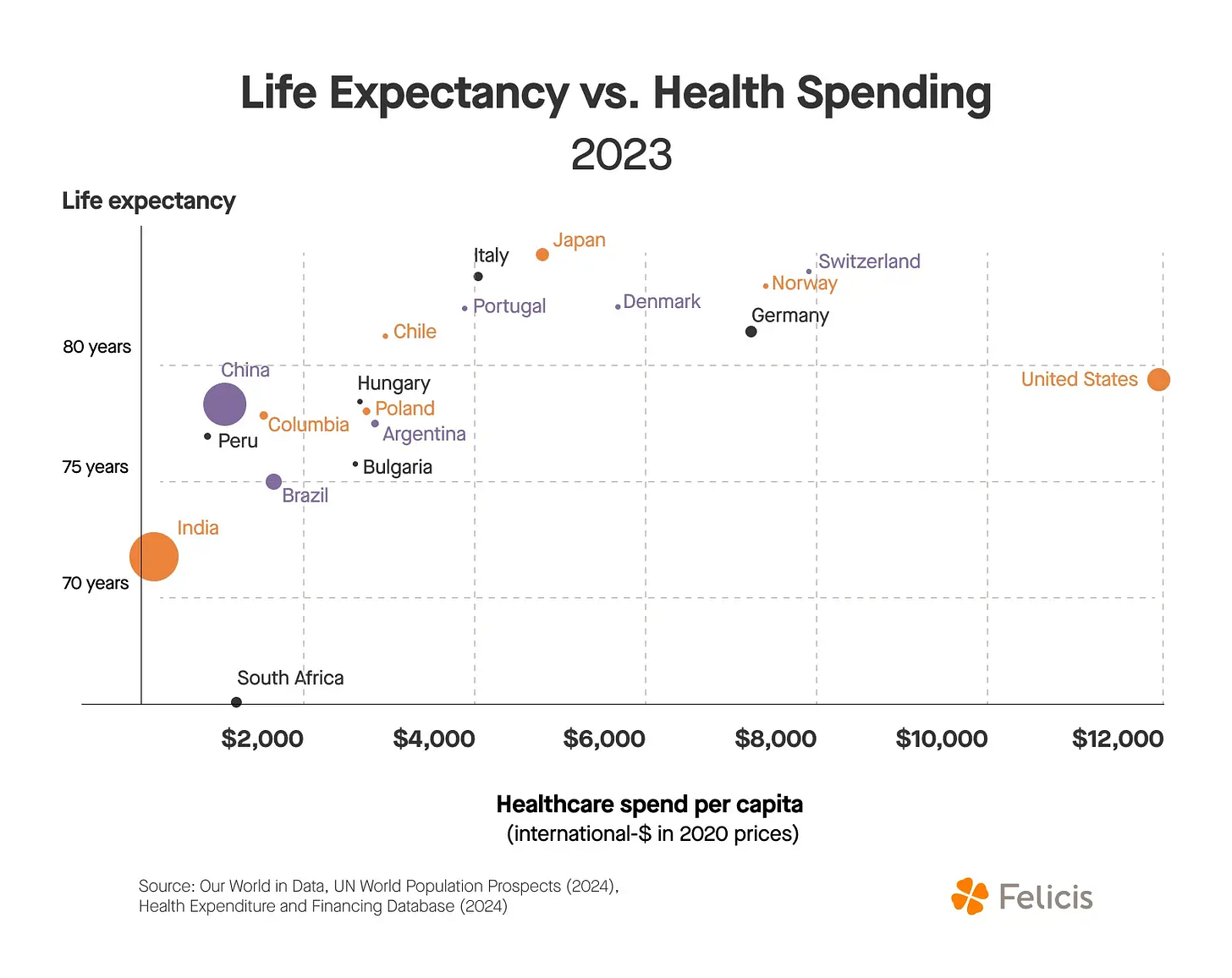
In Part I, we covered why the US healthcare system is so expensive. Over the last 50 years, incentives have led to a system of powerful middlemen, each taking their cut from the $5T spent on healthcare in the US annually. The complex relationships between the players involved (patients, providers, insurance companies, PBMs, pharma, and the US gov’t) lead to intense scrutiny over everyone getting their “fair share.” Translated, lots of paperwork, lots of bureaucracy, lots of administrative waste:
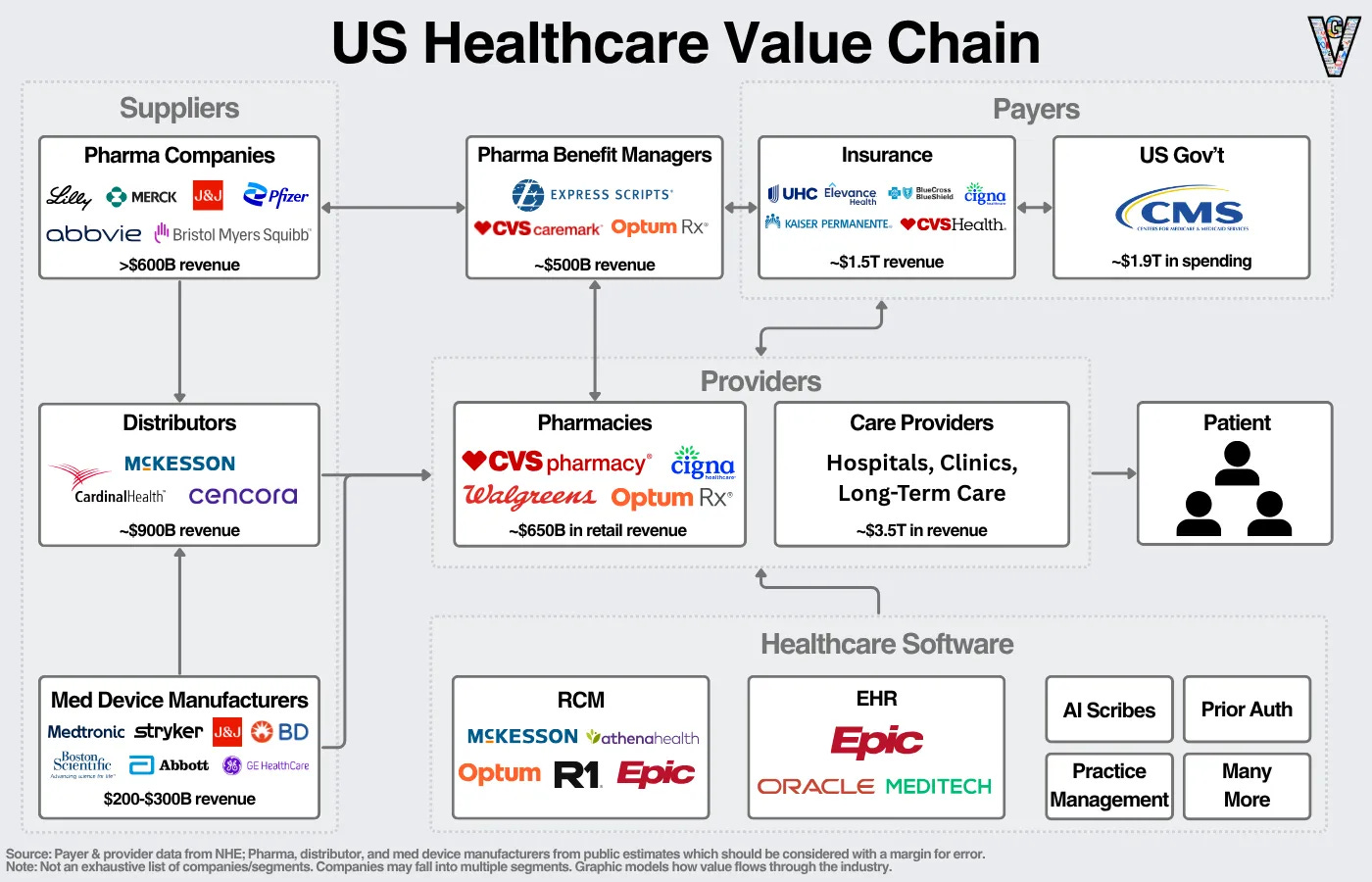
To quantify it, over $1T of admin spend annually…and while we’re much less healthy overall. Full blog from myself and the team at Felicis here:
But when we dig into the details of those administrative tasks, they are text-heavy, voice-heavy, and often straightforward tasks being brute-forced by teams of administrative workers.
They’re calling, emailing, and writing letters to patients, PBMs, insurance companies; many of them spend hours a week faxing documents. We’re talking about AGI, and our largest industry is doing business via fax!
As succinctly as possible, here’s why I’m so excited about the opportunity for healthcare in AI:
This is a critically important problem for our country to solve. No one is satisfied with the system we have today (not patients, not providers, and not payers).
LLMs are perfectly suited to automate MANY of these administrative tasks in healthcare. Great companies resemble the technology waves they ride in on.
If a company can break in, the moats in healthcare are incredible. Of Epic’s over 600 customers, they’ve never lost a single one.
Finally, any meaningful improvement in efficiency creates a massive business opportunity. When you’re tackling a (literal) trillion-dollar problem (seriously, it’s literally a trillion dollars of spend, this is not VC talk for the ‘next trillion dollar company’), any meaningful % improvement can create a very large opportunity.
This article focuses primarily on the administrative applications of AI in healthcare, there are many others that are outside the scope of this article today. To be clear: this will not be easy. AI will not “solve” everything. There are two paths to fix this problem: reform the system or play within the bounds of the system today. As a technologist and investor, I choose the latter.
II. The State of Healthcare Software Today
Before we can even START to talk about AI’s impact, we have to understand two topics:
The healthcare software landscape today
Why its impact has been limited
The healthcare software landscape today
Given our focus on AI in healthcare today, I don’t want to bog you down with an exhaustive list of companies. I’ll point out the largest healthcare software companies:
The biggest categories are the healthcare systems of record:
EHRs (electronic health records): storage of patient medical records
RCMs (revenue cycle managment): manages the billing process between payers, providers, and patients
PMSs (practice management software): manages scheduling, billing, AND EHRs for smaller clinics
But you may notice: wait, these companies are kind of small relative to healthcare, a $5T industry? Yes! Epic, the healthcare giant, only has $5B in revenue?
It points to an unfortunate fact that those in healthcare know well: healthcare software’s impact has been relatively limited in both dollars and automation.
Why has healthcare software’s impact been limited?
I want to lay out very clearly why its impact has been limited AND why it changes now:
1. Data in healthcare is nuanced, and can’t be forced into an objective system
Remember how I was talking about all parties wanting their “fair share” and the ensuing documentation requirements because of that?
Well, the big problem with that is it forces nuanced, unstructured healthcare data into a structured format. Every patient interaction has to be translated to one of thousands of medical codes, turned into a bill, and justified to insurance on why the final diagnosis/prescription was made.
Ask any physician, and they’ll tell you: it’s not so simple.
All this did was force a burden on clinicians to take copious notes, put them into the EHR, and then be forced to justify their notes/prescriptions for any questions/issues from insurance (and there are a lot of them).
This work couldn’t be effectively documented and certainly not automated before AI. LLMs change that.
LLMs are wonderful for understanding nuanced, unstructured data, and they create the ability to start to automate these workflows.
2. Healthcare providers have (rightfully) been slow adopters of technology
Providers have been slow to adopt software for three more reasons:
Low profits = low budgets
Low fault-tolerance (i.e., mistakes are costly) = high barrier to adoption
Integration complexity = higher costs, lower adoption.
Today, low budgets are actually a tailwind. Providers told me they have to cut costs to survive, and AI is a really good way to cut costs. Companies are taking spend from labor budgets, not just software budgets, to pay for AI tools. This expands the software market a lot.
Second, fault tolerance is a real concern, but is much higher in administrative workflows where mistakes are already made all the time.
Finally, integration complexity is still an issue. Because healthcare systems are complex, they have complex technology stacks, which further cements switching costs, making adopting new technology more expensive.
Healthcare AI companies and startups must solve this problem themselves. They must take a page out of Palantir’s playbook with the Forward-Deployed-Engineer model where their team goes in to healthcare systems and builds out the integrations required to successfully adopt this software.
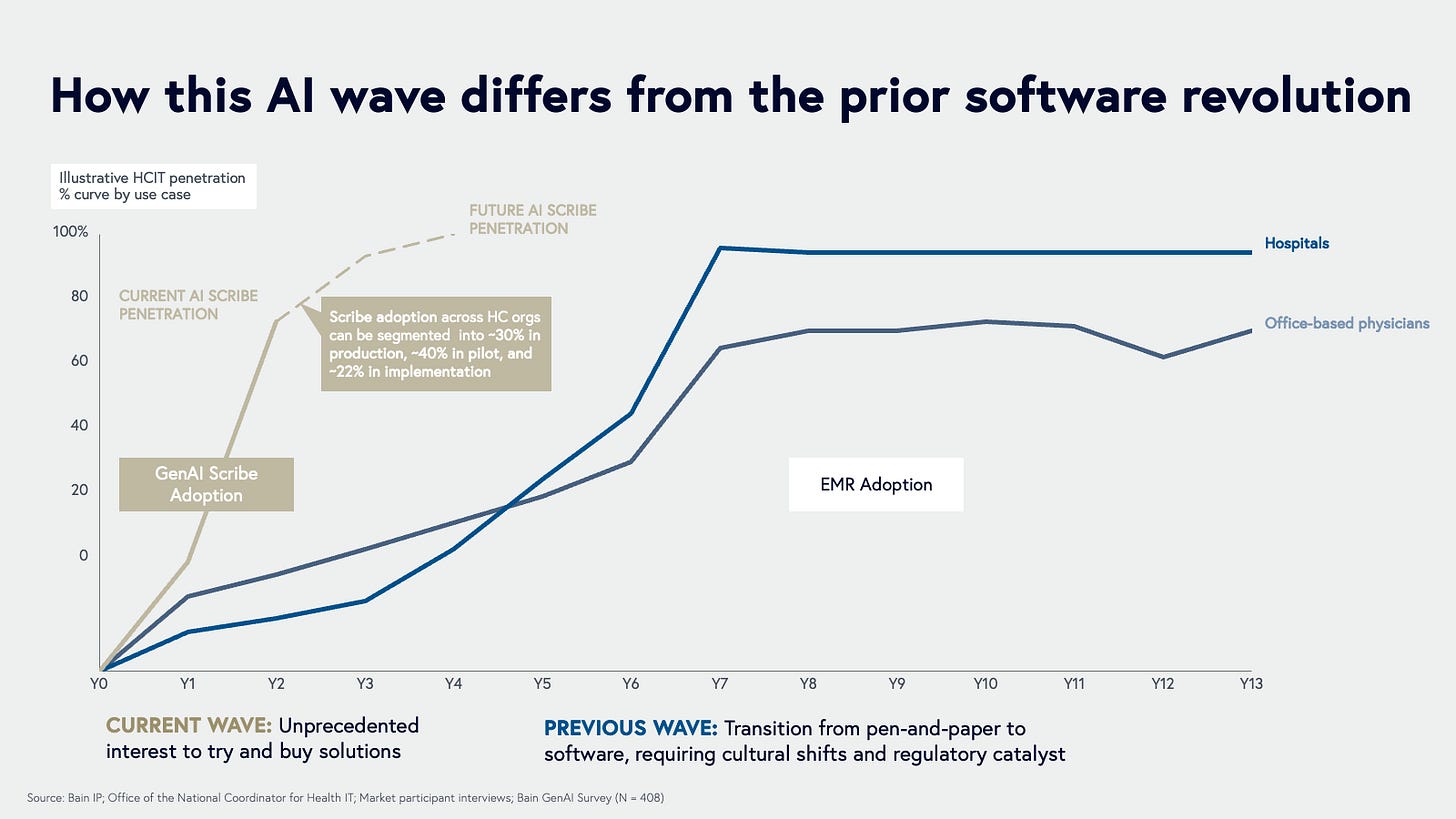
In summary, LLMs ability to actually automate workflows, deliver ROI in the form of cost savings, and a new model for delivering software create a new age of healthcare software opportunities.
As one source told me,”Providers were basically impossible to sell into two years ago, and that’s completely changed.”
III. Where AI is Helping Healthcare’s Administrative Burden
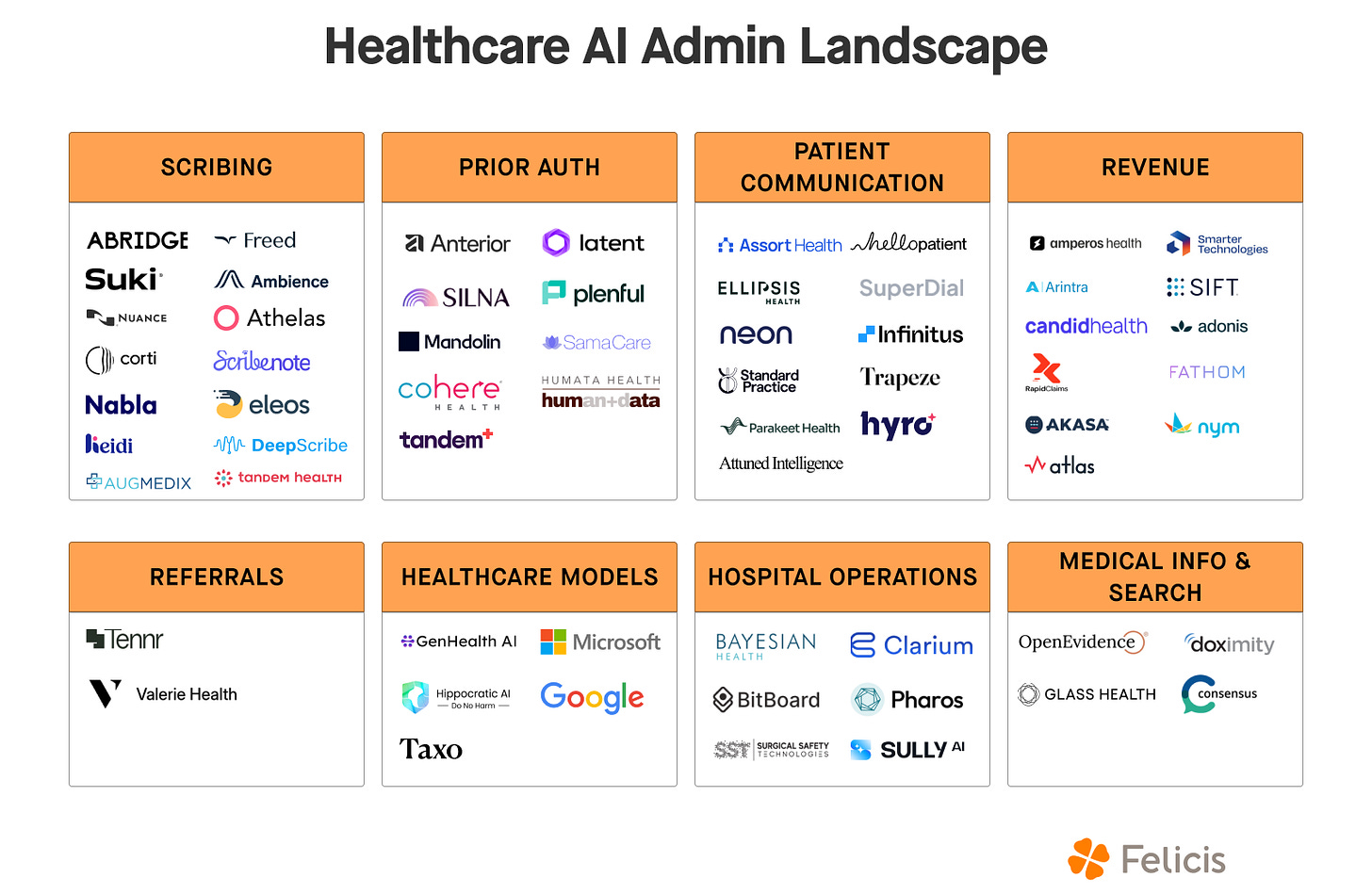
I’m not kidding when I say there’s another task that can be automated around every corner in healthcare. From my research, I came across five key categories of workflows that take up the most time and effort from healthcare providers. See the startups taking on those categories (with a few others) below:
To illustrate AI’s impact today, we can essentially walk through every single step of the healthcare process:
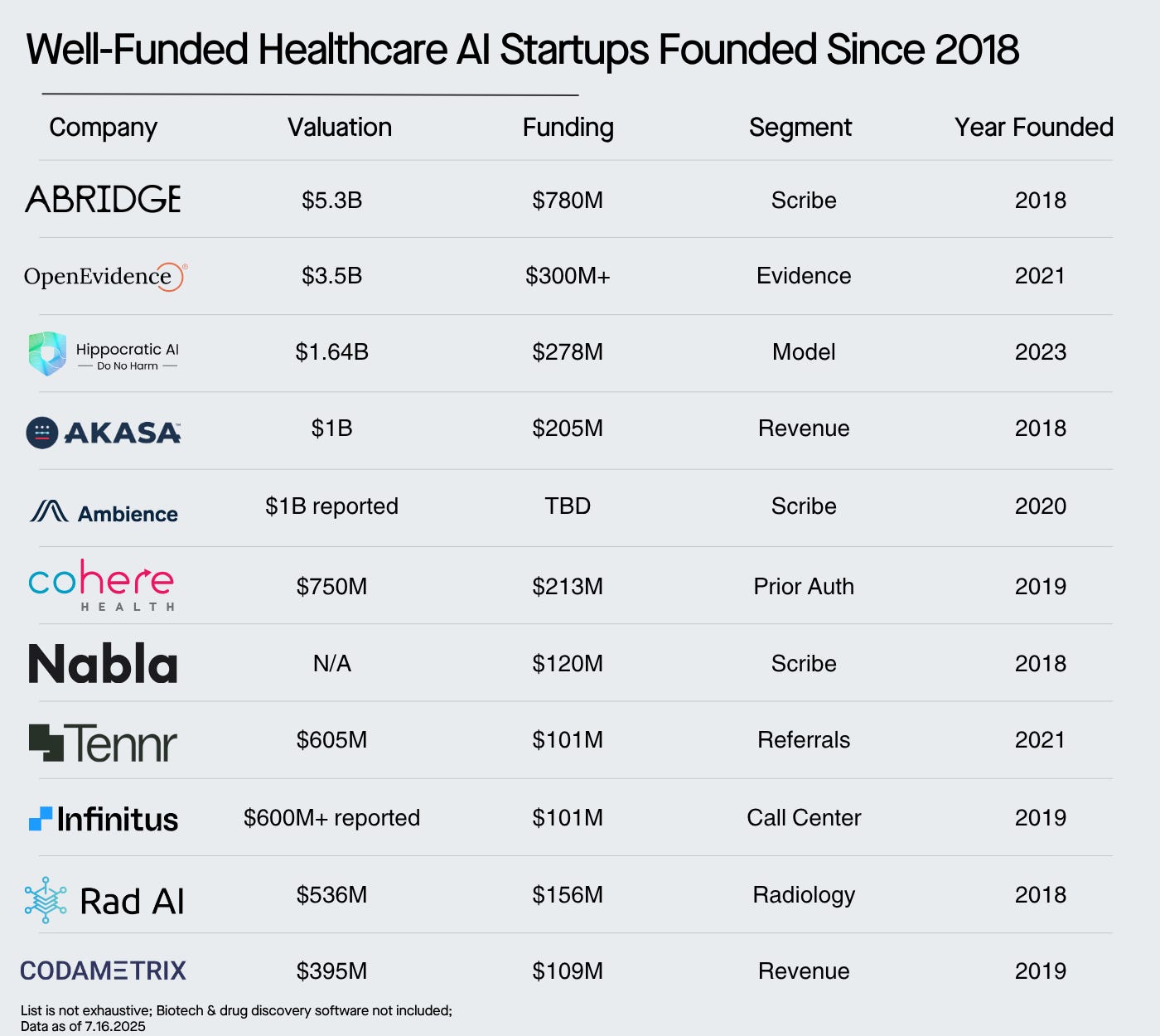
Scribing: Starting with the patient visit, AI scribes take notes for clinicians so that they can focus on engaging with the patient. Abridge is now valued at $5B, and two other unicorns have been created in the scribing market. When I talk about AI being adopted way faster in healthcare than any previous software, this is what I’m talking about.
Some estimates have the % of hospitals using or testing scribes at over 80%:
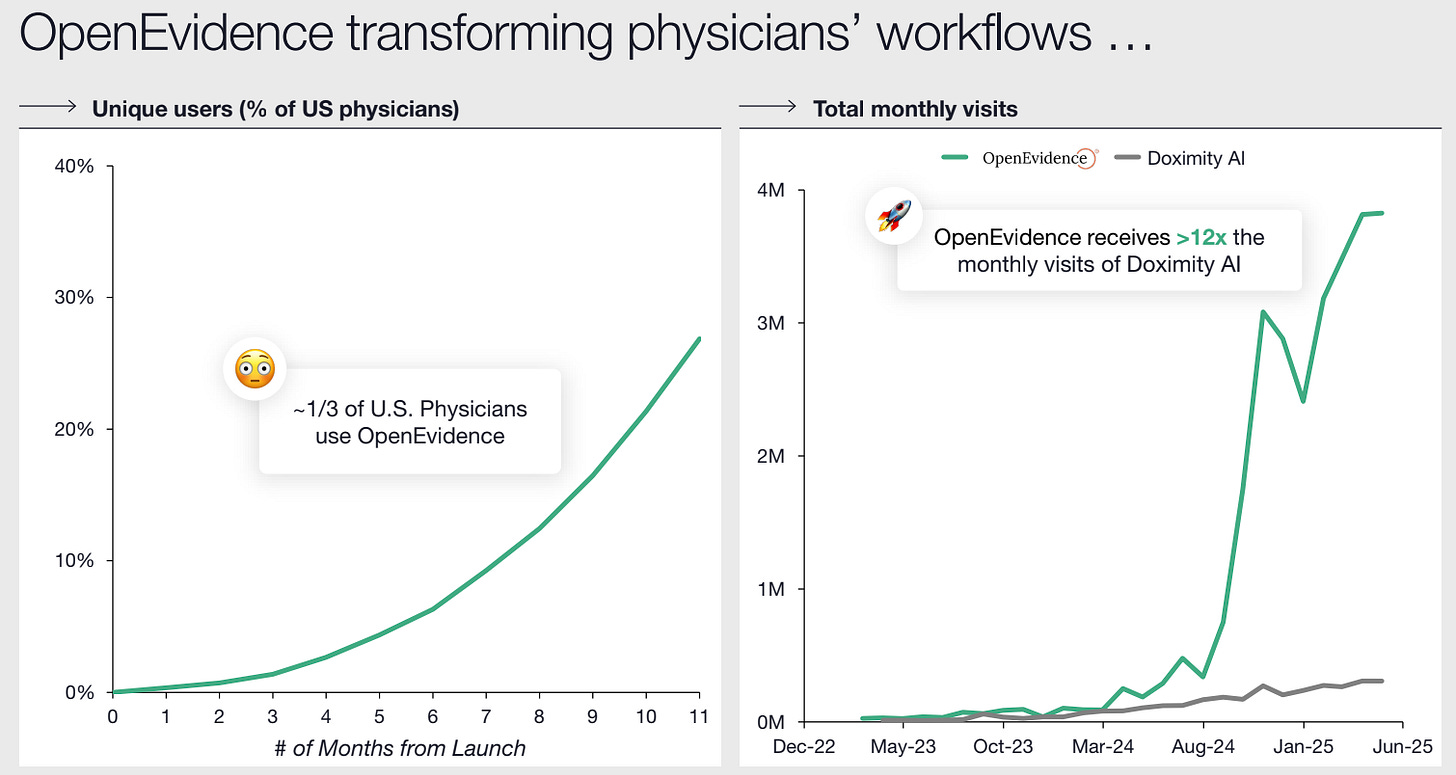
Medical Search: Once the doctor’s seen the patient, they need to do research to come up with a diagnosis. Previously, this was using antiquated medical search tools or Google. Now, many are using AI search tools, led by OpenEvidence, who just raised at a $3.5B valuation.
Over 1/3rd of US physicians are using OpenEvidence 12 months after launch:
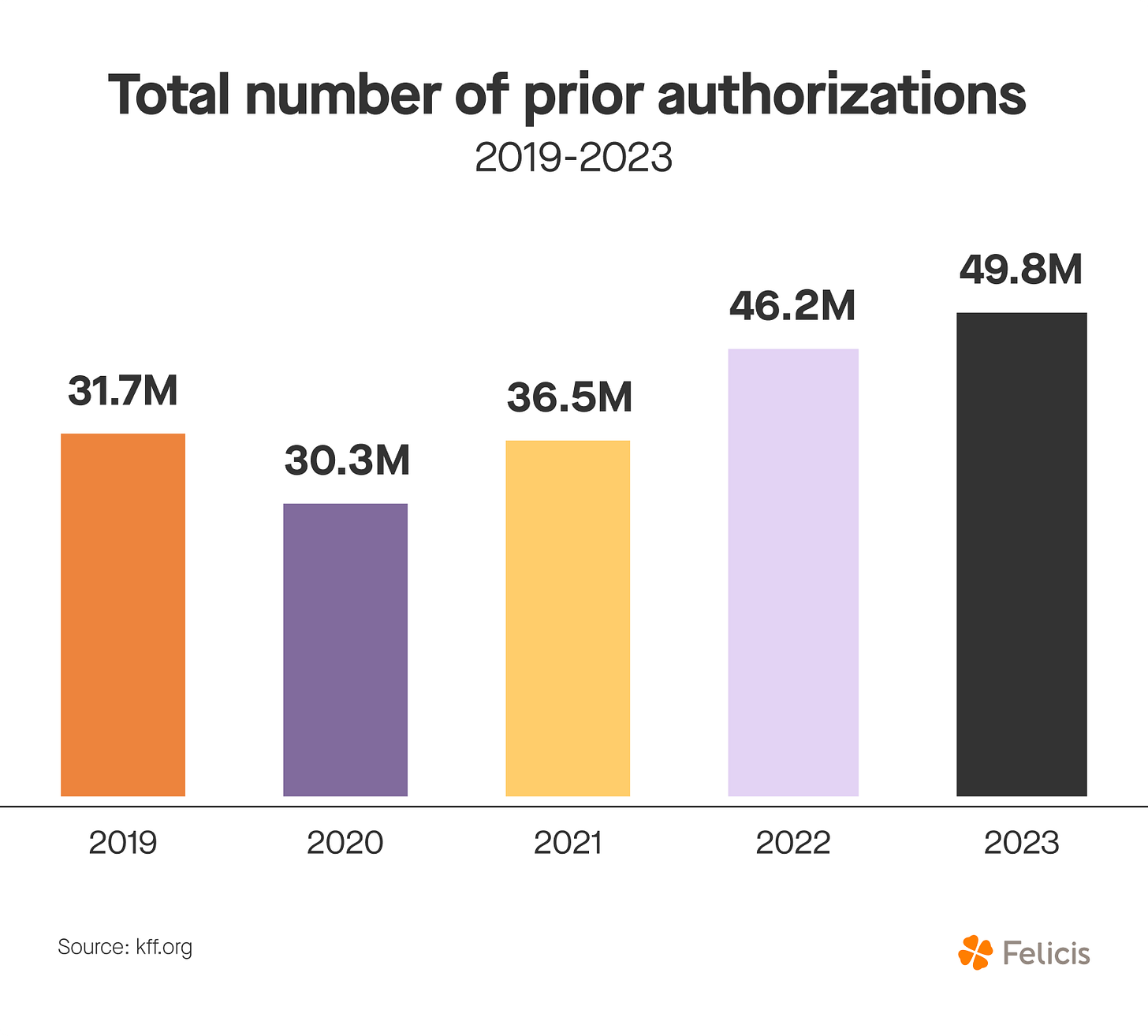
Prior Authorizations: After a diagnosis has been made, many medications or procedures require prior authorizations. Essentially, if insurance doesn’t explicitly cover a prescription or procedure, the provider needs to get pre-approved for insurance. This can be done through prior auth portals, phone calls, and god forbid fax machines.
There are entire PA teams in hospitals just doing prior auths all day long, mistakes are frequently made, and doctors get pulled in to help fix them. It’s the quintessential highly painful + very common workflow that AI is automating.
Revenue Cycle Operations: Once a procedure is complete, that clinical note needs to be translated to medical codes (of which, there are about 70k). That code is translated to a bill/claim, and sent to insurance, who approves or denies it.
Insurance companies are automating claims processing, or reviewing of the claim. If it’s denied, the provider appeals it, which is likely overturned. (And many providers are using AI to write appeals letters now).
After all that, a bill is sent to the patient.
Customer Service: Finally, if the patient wants to ask questions, schedule a follow-up, or pay a bill, they’ve got to call the provider. The majority of basic questions can now be automated with AI. Essentially, immediately cutting spend and improving patient satisfaction with AI.
All five of these categories of administrative spend are centered around voice and text, that AI can now automate, and it’s why we’ve seen such rapid adoption of these tools.
All in all, we’ve already seen large, well-funded companies emerge in all of these categories:
To be clear, there are MANY other companies in each of these categories, this is just illustrative of the excitement from both investors and customers for these solutions.
IV. The Path Ahead: How to Maximize Impact on the Healthcare System
So, early demand is there, the impact in several categories is already being seen. How do we ensure this is a sustainable trend in both (1) building enduring companies and (2) ensure those companies maximize their impact?
I see three paths to do so:
1. Early point solutions need to expand as platforms.
In my Toast Deep Dive, I laid out the path to go from owning a workflow -> being a system of record. When I wrote that, I had Abridge in the back of my mind. Once you own the clinical note, you can now automate the key workflows around that clinical note, build a platform, and expand to become a system of record.
In Abridge’s case (and other AI scribes), you can take the clinical note, automatically translate that to a medical code and claim, send that to insurance, and expand to own the workflows around revenue cycle management.
For the investors at the $5B valuation, this is likely the vision they see.
2. Companies need to scale GTM as quickly as possible
To maximize their impact, companies to maximize their reach. Time for capitalism to shine!
I’ve exhaustively covered the Power Law on this publication. If there’s one applicable lesson from it, you have to start your power law compounding as quickly as possible.
This means whoever moves fastest often wins the mindshare of customers, the mindshare of investors, and creates a flywheel of increasing returns. The goal is to get that flywheel turning as quickly as possible, either through:
Early traction (either sheer volume or top-tier customers)
Fundraising (again through amount or top-tier customers)
Marketing (owning mindshare)
All of these variables then compound on each other.
3. Leverage this newly automated data to improve more than just efficiency, but make a real impact on patient outcomes
Many clinicians I talked to about this problem were completely uninterested in the admin side of workflows. They were obsessed with creating better outcomes for patients.
The fact that OpenEvidence already supports 1/3rd of US physicians less than 12 months after launching is incredible.
But as we aggregate more and more data, the ability to positive affect patient outcomes improves as well.
In a perfect world, we’ll have the ability to aggregate much of the (now automated) data from AI scribes into one database so that every single symptom -> diagnosis is tracked in the US. As the dataset grows and models get better, we’ll get faster and faster diagnoses.
Hopefully, we’ll leave a world behind someone has to bounce around between ten specialists before getting a diagnosis for a rare disease.
One final thought on the exciting thing about boring things.
Prior auths, medical coding, scribing…these processes themselves are boring. But the impact of automating these tasks is not.
As we think about the economic impact of AI, much of it will come down to tasks like scribing and prior authorizations.
Nobody wants to do them, it’s routine work, and so we’ll hand it off to AI. It makes the economy more productive, very few will notice; and in aggregate, it will make us meaningfully more productive.
In the process, it will help fix one of our most important and most broken systems. And one that MUST be solved for the US to thrive moving forward. And that’s something to get very excited about.
As always, thanks for reading!
Disclaimer #2: The information contained in this article is not investment advice and should not be used as such. Investors should do their own due diligence before investing in any securities discussed in this article. While I strive for accuracy, I can’t guarantee the accuracy or reliability of this information. This article is based on my opinions and should be considered as such, not a point of fact. Views expressed in posts and other content linked on this website or posted to social media and other platforms are my own and are not the views of Felicis Ventures Management Company, LLC.



Interesting!
Great one!